Brand Name
Agrylin
Generic Name
Anagrelide
View Brand Information FDA approval date: March 14, 1997
Classification: Platelet-reducing Agent
Form: Capsule
What is Agrylin (Anagrelide)?
Anagrelide capsules are indicated for the treatment of patients with thrombocythemia, secondary to myeloproliferative neoplasms, to reduce the elevated platelet count and the risk of thrombosis and to ameliorate associated symptoms including thrombo-hemorrhagic events. Anagrelide is a platelet reducing agent indicated for the treatment of thrombocythemia, secondary to myeloproliferative neoplasms, to reduce the elevated platelet count and the risk of thrombosis and to ameliorate associated symptoms including thrombo-hemorrhagic events.
Approved To Treat
Top Local Experts
There are no experts for this drug
Related Clinical Trials
A Phase 3, Randomized, Open-label, Active-Comparator-Controlled Clinical Study to Evaluate the Safety and Efficacy of Bomedemstat (MK-3543/IMG-7289) Versus Best Available Therapy (BAT) in Participants With Essential Thrombocythemia Who Have an Inadequate Response to or Are Intolerant of Hydroxyurea
Summary: This is a study evaluating the safety and efficacy of bomedemstat (MK-3543) compared with the best available therapy (BAT) in participants with essential thrombocythemia (ET) who have an inadequate response to or are intolerant of hydroxyurea. The primary study hypothesis is that bomedemstat is superior to the best available therapy with respect to durable clinicohematologic response (DCHR).
Related Latest Advances
Brand Information
Agrylin (anagrelide hydrochloride)
1INDICATIONS AND USAGE
AGRYLIN is indicated for the treatment of patients with thrombocythemia, secondary to myeloproliferative neoplasms, to reduce the elevated platelet count and the risk of thrombosis and to ameliorate associated symptoms including thrombo-hemorrhagic events.
2DOSAGE AND ADMINISTRATION
2.1Recommended Starting Dosage
2.2Dose Titration Based Upon Platelet Response
Continue the starting dose for at least one week and then titrate to reduce and maintain the platelet count below 600,000/µL, and ideally between 150,000/µL and 400,000/µL. The dose increment should not exceed 0.5 mg/day in any one week. Dosage should not exceed 10 mg/day or 2.5 mg in a single dose. Most patients will experience an adequate response at a dose of 1.5 to 3.0 mg/day. Monitor platelet counts weekly during titration then monthly or as necessary.
2.3Dose Modifications for Hepatic Impairment
In patients with moderate hepatic impairment (Child Pugh score 7-9) start AGRYLIN therapy at a dose of 0.5 mg/day and monitor frequently for cardiovascular events [see Warnings and Precautions (5.1), Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)]. Patients with moderate hepatic impairment who have tolerated AGRYLIN therapy for one week may have their dose increased. The dose increase increment should not exceed 0.5 mg/day in any one week. Avoid use of AGRYLIN in patients with severe hepatic impairment.
2.4Clinical Monitoring
AGRYLIN therapy requires clinical monitoring, including complete blood counts, assessment of hepatic and renal function, and electrolytes.
To prevent the occurrence of thrombocytopenia, monitor platelet counts every two days during the first week of treatment and at least weekly thereafter until the maintenance dosage is reached. Typically, platelet counts begin to respond within 7 to 14 days at the proper dosage. In the clinical trials, the time to complete response, defined as platelet count ≤600,000/µL, ranged from 4 to 12 weeks. In the event of dosage interruption or treatment withdrawal, the rebound in platelet count is variable, but platelet counts typically will start to rise within 4 days and return to baseline levels in one to two weeks, possibly rebounding above baseline values. Monitor platelet counts frequently.
3DOSAGE FORMS AND STRENGTHS
Capsules: White, opaque capsule, imprinted with " 063" in black ink. Each capsule contains 0.5 mg anagrelide equivalent to 0.61 mg anagrelide hydrochloride USP.
063" in black ink. Each capsule contains 0.5 mg anagrelide equivalent to 0.61 mg anagrelide hydrochloride USP.
 063" in black ink. Each capsule contains 0.5 mg anagrelide equivalent to 0.61 mg anagrelide hydrochloride USP.
063" in black ink. Each capsule contains 0.5 mg anagrelide equivalent to 0.61 mg anagrelide hydrochloride USP.4CONTRAINDICATIONS
None.
5CONTRAINDICATIONS
None.
6WARNINGS AND PRECAUTIONS
6.1Cardiovascular Toxicity
Torsades de pointes and ventricular tachycardia have been reported with AGRYLIN. Obtain a pre-treatment cardiovascular examination including an ECG in all patients. During treatment with AGRYLIN monitor patients for cardiovascular effects and evaluate as necessary.
AGRYLIN increases the QTc interval of the electrocardiogram and increases the heart rate in healthy volunteers [see Clinical Pharmacology (12.2)].
Do not use AGRYLIN in patients with known risk factors for QT interval prolongation, such as congenital long QT syndrome, a known history of acquired QTc prolongation, medicinal products that can prolong QTc interval and hypokalemia [see Drug Interactions (7.1)].
Hepatic impairment increases anagrelide exposure and could increase the risk of QTc prolongation. Monitor patients with hepatic impairment for QTc prolongation and other cardiovascular adverse reactions. The potential risks and benefits of AGRYLIN therapy in a patient with mild and moderate hepatic impairment should be assessed before treatment is commenced. Reduce AGRYLIN dose in patients with moderate hepatic impairment. Avoid use of AGRYLIN in patients with severe hepatic impairment.
In patients with heart failure, bradyarrhythmias, or electrolyte abnormalities, consider periodic monitoring with electrocardiograms [see Clinical Pharmacology (12.2)].
AGRYLIN is a phosphodiesterase 3 (PDE3) inhibitor and may cause vasodilation, tachycardia, palpitations, and congestive heart failure. Other drugs that inhibit PDE3 have caused decreased survival when compared with placebo in patients with Class III-IV congestive heart failure [see Drug Interactions (7.2)].
In patients with cardiac disease, use AGRYLIN only when the benefits outweigh the risks.
6.2Pulmonary Hypertension
Cases of pulmonary hypertension have been reported in patients treated with AGRYLIN. Evaluate patients for signs and symptoms of underlying cardiopulmonary disease prior to initiating and during AGRYLIN therapy [see Adverse Reactions (6.1)].
6.3Bleeding Risk
Use of concomitant AGRYLIN and aspirin increased major hemorrhagic events in a postmarketing study. Assess the potential risks and benefits for concomitant use of AGRYLIN with aspirin, since bleeding risks may be increased. Monitor patients for bleeding, including those receiving concomitant therapy with other drugs known to cause bleeding (e.g., anticoagulants, PDE3 inhibitors, NSAIDs, antiplatelet agents, selective serotonin reuptake inhibitors) [see Drug Interactions (7.3), Clinical Pharmacology (12.3)].
6.4Pulmonary Toxicity
Interstitial lung diseases (including allergic alveolitis, eosinophilic pneumonia and interstitial pneumonitis) have been reported to be associated with the use of AGRYLIN in post-marketing reports. Most cases presented with progressive dyspnea with lung infiltrations. The time of onset ranged from 1 week to several years after initiating AGRYLIN. If suspected, discontinue AGRYLIN and evaluate. Symptoms may improve after discontinuation [see Adverse Reactions (6)].
7ADVERSE REACTIONS
The following clinically significant adverse reactions are discussed in greater detail in other sections of the labeling:
- Cardiovascular Toxicity [see Warnings and Precautions (5.1)]
- Pulmonary Hypertension [see Warnings and Precautions (5.2)]
- Bleeding Risk [see Warnings and Precautions (5.3)]
- Pulmonary Toxicity [see Warnings and Precautions (5.4)]
7.1Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
7.2Postmarketing Experience
The following adverse reactions have been identified during post-marketing use of AGRYLIN. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Cardiac disorders: Prinzmetal angina, Torsades de pointes.
Respiratory, thoracic, and mediastinal disorders: Interstitial lung diseases (including allergic alveolitis, eosinophilic pneumonia, and interstitial pneumonitis) [see Warnings and Precautions (5.4)].
Renal and urinary disorders: Tubulointerstitial nephritis.
Hepatobiliary disorders: Clinically significant hepatotoxicity (including symptomatic ALT and AST elevations and elevations greater than three times the ULN).
Nervous system disorders: Cerebral infarction
Other adverse reactions in pediatric patients reported in spontaneous reports and literature reviews include:
Blood and lymphatic system disorders: Anemia.
Skin and subcutaneous tissue disorders: Cutaneous photosensitivity.
Investigations: Elevated leukocyte count.
8DRUG INTERACTIONS
8.1Drugs that Prolong QT
Avoid use of AGRYLIN in patients taking medications that may prolong QT interval (including, but not limited to, chloroquine, clarithromycin, haloperidol, methadone, moxifloxacin, amiodarone, disopyramide, procainamide, and pimozide) [see Warnings and Precautions (5.1) and Clinical Pharmacology (12.2)].
8.2PDE3 Inhibitors
AGRYLIN is a phosphodiesterase 3 (PDE3) inhibitor. Avoid use of drug products with similar properties such as inotropes and other PDE3 inhibitors (e.g., cilostazol, milrinone) [see Warnings and Precautions (5.1) and Clinical Pharmacology (12.2)].
8.3Aspirin and Drugs that Increase Bleeding Risk
Co-administration of single-dose or repeat-dose AGRYLIN and aspirin showed greater ex vivo anti-platelet aggregation effects than administration of aspirin alone [see Clinical Pharmacology (12.3)]. Results from an observational study in patients with essential thrombocythemia suggest the rate of major hemorrhagic events (MHEs) in patients treated with AGRYLIN is higher than in those subjects treated with another cytoreductive treatment. The majority of the major hemorrhagic events occurred in patients who were also receiving concomitant anti-aggregatory treatment (primarily, aspirin). Therefore, the potential risks of the concomitant use of AGRYLIN with aspirin should be assessed, particularly in patients with a high-risk profile for hemorrhage, before treatment is initiated [see Warnings and Precautions (5.3)].
Monitor patients for bleeding, particularly those receiving concomitant therapy with other drugs known to cause bleeding (e.g., anticoagulants, PDE3 inhibitors, NSAIDs, antiplatelet agents, selective serotonin reuptake inhibitors).
8.4CYP450 Interactions
9USE IN SPECIFIC POPULATIONS
9.1Pregnancy
9.2Lactation
9.3Females and Males of Reproductive Potential
9.4Pediatric Use
The safety and effectiveness of AGRYLIN have been established in pediatric patients 7 years of age and older. There are no data for pediatric patients less than 7 years of age. Use of AGRYLIN in these pediatric patients is supported by evidence from adequate and well controlled studies of AGRYLIN in adults with additional pharmacokinetic, pharmacodynamic, and safety data in 18 pediatric patients aged 7 through 16 years with thrombocythemia secondary to ET [see Dosage and Administration (2.1), Clinical Pharmacology (12.3), and Clinical Studies (14)].
There were no apparent trends or differences in the types of adverse events observed between the pediatric patients compared with those of the adult patients [see Adverse Reactions (6.1)].
9.5Geriatric Use
Of the 942 subjects in clinical studies of AGRYLIN, 42.1% were 65 years and over, while 14.9% were 75 years and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in response between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
9.6Hepatic Impairment
Hepatic metabolism is the major route of anagrelide clearance. Exposure to anagrelide is increased 8-fold in patients with moderate hepatic impairment [see Clinical Pharmacology (12.3)] and dose reduction is required [see Dosage and Administration (2.3)]. Use of AGRYLIN in patients with severe hepatic impairment has not been studied. Avoid use of AGRYLIN in patients with severe hepatic impairment. The potential risks and benefits of AGRYLIN therapy in a patient with mild and moderate hepatic impairment should be assessed before treatment is commenced. Assess hepatic function before and during AGRYLIN treatment [see Warnings and Precautions (5.1)].
10OVERDOSAGE
At higher than recommended doses, AGRYLIN has been shown to cause hypotension. There have been postmarketing case reports of intentional overdose with AGRYLIN. Reported symptoms include sinus tachycardia and vomiting. Symptoms resolved with supportive management. Platelet reduction from AGRYLIN therapy is dose-related; therefore, thrombocytopenia, which can potentially cause bleeding, is expected from overdosage.
In case of overdosage, stop AGRYLIN dosing and monitor platelet counts for thrombocytopenia and observe for possible complications such as bleeding. Consider resumption of AGRYLIN dosing once the platelet count returns to the normal range.
11DESCRIPTION
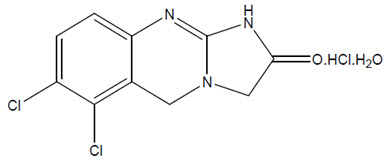
AGRYLIN (anagrelide hydrochloride) is a platelet-reducing agent. Its chemical name is 6,7-dichloro-1,5-dihydroimidazo[2,1-b]quinazolin-2(3H)-one monohydrochloride monohydrate. The molecular formula is C10H7Cl2N3O∙HCl∙H2O which corresponds to a molecular weight of 310.55. The structural formula is:
Anagrelide hydrochloride is an off-white powder. It is very slightly soluble in water and sparingly soluble in dimethyl sulfoxide and dimethylformamide.
AGRYLIN is supplied as capsules for oral administration, containing 0.5 mg of anagrelide (equivalent to 0.61 mg of anagrelide hydrochloride USP). The capsules also contain anhydrous lactose NF, crospovidone NF, lactose monohydrate NF, magnesium stearate NF, microcrystalline cellulose NF, and povidone NF as inactive ingredients. The capsule shell contains gelatin, titanium dioxide, and black iron oxide.
12CLINICAL PHARMACOLOGY
12.1Mechanism of Action
The precise mechanism by which anagrelide reduces blood platelet count is unknown. In cell culture studies, anagrelide suppressed expression of transcription factors including GATA-1 and FOG-1 required for megakaryocytopoiesis, ultimately leading to reduced platelet production.
12.2Pharmacodynamics
In blood withdrawn from normal volunteers treated with anagrelide, a disruption was found in the postmitotic phase of megakaryocyte development and a reduction in megakaryocyte size and ploidy. At therapeutic doses, anagrelide does not produce significant changes in white cell counts or coagulation parameters, and may have a small, but clinically insignificant effect on red cell parameters. The active metabolite, 3-hydroxy anagrelide, has similar potency and efficacy to that of anagrelide in the platelet lowering effect; however, exposure (measured by plasma AUC) to 3-hydroxy anagrelide is approximately 2-fold higher compared to anagrelide. Anagrelide and 3-hydroxy anagrelide inhibit cyclic AMP phosphodiesterase 3 (PDE3) and 3-hydroxy anagrelide is approximately forty times more potent than anagrelide (IC50s = 0.9 and 36 nM, respectively). PDE3 inhibition does not alter platelet production. PDE3 inhibitors, as a class can inhibit platelet aggregation. However, significant inhibition of platelet aggregation is observed only at doses of anagrelide higher than those typically required to reduce platelet count. PDE3 inhibitors have cardiovascular (CV) effects including vasodilation, positive inotropy and chronotropy.
12.3Pharmacokinetics
Dose proportionality has been found in the dose range 0.5 mg to 2.5 mg.
13NONCLINICAL TOXICOLOGY
13.1Carcinogenesis, Mutagenesis, Impairment of Fertility
In a two-year rat carcinogenicity study a higher incidence of uterine adenocarcinoma, relative to controls, was observed in females receiving 30 mg/kg/day (at least 174 times human AUC exposure after a 1 mg twice daily dose). Adrenal pheochromocytomas were increased relative to controls in males receiving 3 mg/kg/day and above, and in females receiving 10 mg/kg/day and above (at least 10 and 18 times respectively human AUC exposure after a 1 mg twice daily dose).
Anagrelide hydrochloride was not mutagenic in the bacterial mutagenesis (Ames) assay or the mouse lymphoma cell (L5178Y, TK+/-) forward mutation assay, and was not clastogenic in the in vitro chromosome aberration assay using human lymphocytes or the in vivo mouse micronucleus test.
Anagrelide hydrochloride at oral doses up to 240 mg/kg/day (233 times the recommended human dose of 10 mg/day based on body surface area) had no effect on fertility and reproductive function of male rats. However, in fertility studies in female rats, oral doses of 30 mg/kg/day (29 times the recommended maximum human dose based on body surface area) or higher resulted in increased pre- and post-implantation loss and a decrease in the number of live embryos.
13.2Animal Toxicology and/or Pharmacology
In the 2-year rat study, a significant increase in non-neoplastic lesions was observed in anagrelide treated males and females in the adrenal (medullary hyperplasia), heart (myocardial hypertrophy and chamber distension), kidney (hydronephrosis, tubular dilation and urothelial hyperplasia), and bone (femur enostosis). Vascular effects were observed in tissues of the pancreas (arteritis/periarteritis, intimal proliferation, and medial hypertrophy), kidney (arteritis/periarteritis, intimal proliferation, and medial hypertrophy), sciatic nerve (vascular mineralization), and testes (tubular atrophy and vascular infarct) in anagrelide-treated males.
14CLINICAL STUDIES
15HOW SUPPLIED/STORAGE AND HANDLING
AGRYLIN is available as:
0.5 mg, opaque, white capsules imprinted "
16PATIENT COUNSELING INFORMATION
- Dose: Tell the patient that their dose will be adjusted on a weekly basis until they are on a dose that lowers their platelets to an appropriate level. This will also help the patient to adjust to common side effects. Tell the patient to contact their doctor if they experience tolerability issues, so the dose or dosing frequency can be adjusted [see Dosage and Administration (2)].
- Cardiovascular effects: Tell the patient to contact a doctor immediately if they experience chest pain, palpitations, or feel their heartbeat is irregular [see Warnings and Precautions (5.1)].
- Risk of Pulmonary Hypertension: Tell the patient to contact a doctor immediately if they experience shortness of breath, swelling in legs or ankles, or lips and skin turn a bluish color [see Warnings and Precautions (5.2)].
- Risk of bleeding: Warn the patient that concomitant aspirin (or other medicines that affect blood clotting) may increase the risk of bleeding. Tell the patient to contact a doctor immediately if they experience signs or symptoms of bleeding (e.g., vomit blood, pass bloody or black stools) or experience unexplained bruising/bruise more easily than usual [see Warnings and Precautions (5.3), Drug Interactions (7.1)].
- Lactation: Advise patients not to breastfeed during treatment with AGRYLIN, and for one week following the last dose [see Use in Specific Populations (8.2)].
- Infertility: Advise females of reproductive potential treatment with AGRYLIN may impair fertility [see Use in Specific Populations (8.3), Nonclinical Toxicology (13.1)].
17PRINCIPAL DISPLAY PANEL - 0.5 mg Capsule Bottle Label
063-01
NDC 54092-063-01
NDC 54092-063-01
Agrylin
(anagrelide) Capsules
Platelet-reducing Agent
(anagrelide) Capsules
Platelet-reducing Agent
100 CAPSULES
Rx only
0.5 mg
Takeda

Save this treatment for later
Not sure about your diagnosis?
Tired of the same old research?